
Practice Model Trends in Medicare Payments Across States and Regions
Ruby L. Hoyem, PhD
Lorraine Jordan, PhD, CRNA, CAE, FAAN
Valentina V. Lukyanova, PhD
Trinidad Legaspi, JD, LLM
Anesthesia delivery models have long been shaped by workforce trends, state and federal regulations, economic incentives driven by reimbursement, and the normative preferences of provider and facility organizations. In recent years, there has been a significant shift toward greater use of more efficient certified registered nurse anesthetist (CRNA)-oriented delivery models observed at the national level Medicare data. However, given the wide range of these factors across states and regions, this shift has likely occurred at an uneven pace. This study analyzes the influence of provider workforce composition and CRNA scope of practice (SOP) regulations on usage of competing types of anesthesia delivery models, including anesthesiologist alone, care team, and undirected CRNA models. Results show that over the period from 2010-2019, anesthesia delivery models utilized under Medicare Part B have become increasingly oriented around the use of CRNAs. However, increases in the care team vs undirected CRNA model are highly uneven and inconsistent across states, even after adjusting for workforce and SOP. Speculation on additional normative or organization-driven reasons for persistent use of inefficient delivery models in some places is offered.
Keywords: anesthesia workforce, Medicare payments, practice models, state trends
Anesthesia practice models involve certified registered nurse anesthetists (CRNAs) and physician anesthesiologists practicing either alone or together, and sometimes anesthesiologist assistants (AAs) practicing under medical direction of physician anesthesiologists. Studies focused on the quality of care have repeatedly shown no significant differences in anesthesia-related mortality or complication rates for various provider types or practice models, while the undirected CRNA model has been demonstrated to be the most cost-effective.1,2 Contentious debates about the quality of competing models continue. However, other factors have largely influenced the choice of delivery model in hospitals in recent years, including the locally available labor market, state policies, preferences of the medical staff, and historical precedent. Emerging trends, including removing scope of practice (SOP) barriers and increasing financial pressures, have favored the more cost-effective CRNA-centric models over the older physician-centric models, including physician anesthesiologists practicing alone, or directing qualified providers using a fixed ratio of physician anesthesiologists to CRNAs or AAs. Data show a clear and significant national shift in patterns of anesthesia delivery to greater use of CRNAs acting without medical direction, along with a marked decline in physician anesthesiologists practicing alone. What is less clear is why there has been such a shift and how different states and regions have varied in adopting these changes.
• Workforce and Regulatory Influences. Key factors contributing to the differential use of practice models include workforce composition factors and SOP as determined by state legislative and regulatory processes. There is wide variation in the anesthesia provider workforce across states, regions, and urban and rural areas. The composition of an available labor market of anesthesia providers in a particular market may be heavily slanted toward one type of provider or the other. A market with small shares of CRNAs will necessarily have larger shares of physician anesthesiologists performing their own cases as opposed to one with larger shares of CRNAs which can support greater use of a care team or undirected CRNAs. One reason for the increasing use of CRNAs, with or without medical direction, may simply be their disproportionate growth in recent years compared with physician anesthesiologists. The most recent estimate by the Bureau of Labor and Statistics for the national rates of employment for CRNAs was 46,540 compared with 37,430 for physician anesthesiologists.6,7 CRNA-oriented anesthesia delivery models in rural areas, including independent practice, are known to predominate due to a lack of available physician anesthesiologists.8–10 A rural area with an anesthesia labor force made primarily of CRNAs is also perhaps likelier to exhibit localized norms and expectations related to independent CRNA practice as the preferred anesthesia delivery model. Conversely, urban areas with greater numbers of physician anesthesiologists may favor physician-centric models by practicing alone or directing CRNAs and AAs, if present. Thirteen states and the District of Columbia currently license AAs, who must practice under the supervision and direction of a physician anesthesiologist. Additionally, AAs practice under physician delegation in two states. Because AAs cannot practice independently, if an AA is involved in a case, the care team model must be utilized to comply with state laws and most reimbursement regulations.
An individual CRNA’s SOP is determined by education and experience as well as local, state, and federal law and organizational policy.11 Federal law governs the current billing regulations for the direction and supervision of Medicare anesthesia service reimbursement based on the practice model. While Medicare provider reimbursement policy pays for fully independent or autonomous CRNA practice, facilities must comply with Medicare Part A Conditions of Participation to receive Medicare facility reimbursement, unless it is in a state that exercised its right to opt-out of this billing requirement. Facilities also implement their own policies through bylaws and management decisions.
• Other Influences. Because CRNAs practice under various team-oriented arrangements but can also work independently, the mere presence of CRNAs does not clearly drive either the use of team-based or undirected CRNA models. Additional factors must be considered to account for the reason directed versus undirected CRNA models are used within a given market environment or facility; these include state and federal regulatory mechanisms and informal norms and organizational preferences. Figure 1 illustrates a conceptual model of factors influencing the choice of competing anesthesia practice models. Attitudinal or cultural traits that drive organizational policies among facilities and payors are difficult to quantitatively measure at a state level. Therefore, the more abstract impact of these factors is illustrated in the diagram as diffuse external influences instead of explicit arrows among measurable terms. Examining differences in practice models across states regarding the available workforce and scope of practice environment can enable a better understanding of how these factors drive practice model patterns. The variation after adjustment for the workforce and regulatory mechanisms can be interpreted as an indication of the other organizational influences that differentially contribute to practice model patterns, such as provider preferences and discriminatory reimbursement policies.
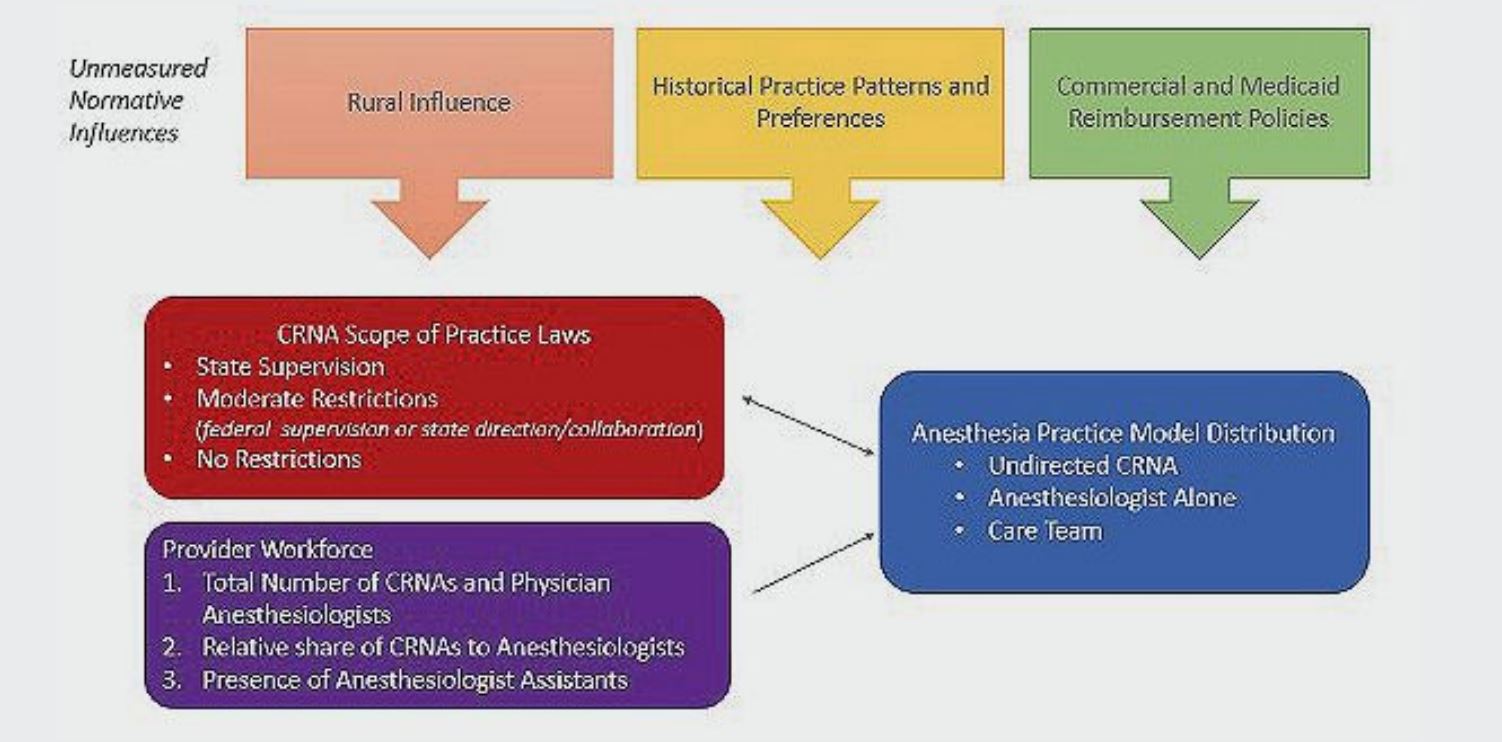
Figure 1. Conceptual Diagram for State-Level Structural Determinants of Anesthesia Practice Model Distribution Abbreviation: CRNA, certified registered nurse anesthetist
MATERIALS AND METHODS
• Data Source. An analysis of anesthesia payment trends was conducted using the Medicare Physician Supplierand Procedure Summary (PSPS) data files from 2010 through 2019. These data represent the calendar year summary of all Part B fee-for-service payments. Data are summarized by a range of claims-based features, including provider specialty, place of service, Carrier ID, Healthcare Common Procedure Coding System code, and modifier. These data were mapped to a state based on the corresponding Carrier ID to obtain a dataset aggregated at the state level.
In the PSPS data files, the regions in the United States are defined based on the geographic divisions used by the Centers for Medicare and Medicaid Services (CMS). CMS divides the United States into four regions:
1) Region 1: northeast (includes the states of Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont).
2) Region 2: midwest (includes the states of Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin).
3) Region 3: south (includes the states of Alabama, Arkansas, Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, West Virginia, and the District of Columbia).
4) Region 4: west (includes the states of Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming).
The primary analysis dataset was further summarized across state, year, and practice model. The dataset includes all anesthesia payments with an initial AA, QK, QY, QZ, AD, or QX modifier. The payments in this dataset reflect over 99.8% of all anesthesia payments in the original files based on the Berenson-Eggers type of service classification. Practice models were defined based on billing modifier with physician anesthesiologist alone including AA, undirected CRNA including QZ, and the care team including all others. The data were aggregated by year, state, and practice model to examine trends across states and regions over time in the changing distribution of practice models. A measure for the share of payments in a state attributed to AAs was calculated by summarizing the total payments associated with AAs for those states and the years where they were authorized to create a measure of the percent of total payments associated with AAs. Because of potential inaccuracies related to administrative data, some states without AA authorization exhibited small amounts of payments for AA services, which were zeroed out.
Provider data used in regression models were derived from the Area Health Resource Files and aggregated to the state level from 2010 to 2019. Calculated measures of anesthesia provider workforce included total providers per 10,000 population and the ratio of CRNAs to physician anesthesiologists. The measure of state-level scope of practice status was based on the American Association of Nurse Anesthesiology classifications of state regulations on CRNA SOP and federal opt-out status. Categories are defined based on:
1) The presence of a supervision requirement in state regulations, which implies a non–opt-out state. Under this requirement, CRNAs have limited or restricted practice authority and must work under the direct supervision of a physician and means that a physician must be physically present during the provision of anesthesia services by the CRNA. The physician does not necessarily have to be an anesthesiologist.
2) The presence of a Direction or Collaboration requirement in state regulations or retention of the federal supervision requirement. Under this category, CRNAs are required to work under the supervision, collaboration, or direction of a physician. The specific level of supervision can vary, ranging from direct physician supervision to a more indirect relationship where a physician is available for consultation if needed. CRNAs evaluate patients, administer anesthesia, and make independent decisions regarding patient care.
3) No state or federal restrictions on SOP. Under this requirement, CRNAs have the authority to practice to the full extent of their education and training without the requirement for physician supervision.
The 2020–2021 regulatory changes in Arizona, Oklahoma, Arkansas, and Michigan fall outside the analysis period and are not reflected.
• Analysis. Descriptive analysis by state and region was conducted to assess overall variation and trends over time in practice models, the provider workforce measures, and CRNA SOP. Practice model choice was then regressed on state-level workforce composition measures and SOP using the summarized data. The model was based on a logistic approach that approximated the distribution of Medicare expenditures across practice models including physician anesthesiologist alone, undirected CRNA, and care team assuming a multinomial distribution. The outcome was represented as the practice model category with aggregated payments specified as a weight variable. State-year level workforce and SOP measures were modeled as dependent variables. Clustering was incorporated at the state level to account for the statelevel aggregation and corresponding correlation in the errors. All analyses were conducted using SAS 9.4 (SAS Institute, Cary NC).
Substantial normative and organizational factors that impact practice models are not included in the model because of significant barriers in measuring such effects. Therefore, a comparative analysis of the differences between the predicted values estimated bythe model and the actual values is conducted to assess
discrepancies across states and regions. The degree of
disparity between the actual share of payments and the
estimated value after adjusting for structural factors
including the composition of providers, availability of
AAs, and state SOP is theorized to represent the degree
to which delivery models are determined by normative
preferences of providers and facilities based on historical patterns or the presence of other influential market
factors such as reimbursement policies that favor one
type of model or another.
RESULTS
• Regional Shifts in Practice Models, Provider Composition, and Scope of Practice. Descriptive findings illustrate the changing practice environment across regions with regard to the types of providers composing the labor force and the anesthesia practice models in use. Figure 2 presents a set of maps comparing the share of each anesthesia delivery model by state in 2019. There is significant state variation for each model. The share of QZ payments for undirected CRNA services ranges from < 10% across most of the northeast to > 85% in Arkansas and Idaho. The share of AA for physician anesthesiologists practicing alone ranges from < 5% in the upper Midwest to > 80% in many western states and > 60% in New York, New Jersey, and Indiana. The care team or the medical direction model includes the physician modifiers QK for 1:2–4, QY for 1:1, and AD for supervision of 1:> 4, along with the QX for the CRNA or anesthesiologist assistant. The share of this practice model ranges from < 15% across virtually all western states to over 70% in Minnesota, Pennsylvania, Delaware, and West Virginia.
Nationally, the share of CRNAs in the anesthesia provider labor force shifted by 7 points between 2010 and 2019 to > 52% resulting in an increase in the ratio of CRNAs to physician anesthesiologists of 0.84 to 1.11, as seen in Table 1. A similar shift occurred in all regions. However, in the south and midwest, the ratio of CRNAs to physician anesthesiologists has reached 1.5, while in the northeast and west, the ratio remains well below 1.0 at 0.81 and 0.45, respectively. Across the country, the workforce has seen an increase in providers per capita, with the midwest, south, and sortheast all having a similar density of providers ranging from 3.26–3.34 per 10,000 population. The west, by contrast, has only 2.11 providers per 10,000 population. The level of AA participation remains quite low, with only Georgia and Vermont having > 5% of Medicare payments attributed to AAs (state level results are presented in Appendix A). Nationally, in the 15 states and the District of Columbia where AAs are practicing, payments for AA services represent only 3.65% of all Medicare reimbursement. Three states have relaxed or removed CRNA SOP restrictions period. Minnesota, which opted out of federal supervision prior to 2010, removed its requirement for direction/collaboration in 2014; Delaware removed its state supervision requirement in 2014 but retained the federal requirement; and Kentucky opted out in 2012 and removed its direction/collaboration restriction in 2018.
Figure 3 illustrates the shift in practice model usage from 2010–2019 for each state sorted by region. The data exhibit a clear regional pattern. Nearly all states exhibit a shift away from the use of the physician anesthesiologist-alone model. Yet they vary to some degree in the shift toward the care team or undirected CRNA model. In the west, where the share of physicians in the anesthesia labor force is high and there has traditionally been an aversion to team-based care models, this shift is primarily toward the undirected CRNA model.
Conversely, in the northeast, the shift has been smaller and primarily toward greater use of the care team model, while the share of undirected CRNA payments remains low. In the south and midwest, there has been significant shift toward the use of the undirected CRNA model and away from the physician anesthesiologist-alone model or the care team model, depending on the state. New Mexico, Louisiana, Mississippi, Tennessee, and Oklahoma have seen the largest increases in using of the undirected CRNA model. Some states in both these regions, including Wisconsin, Illinois, and Maryland, have also seen significant growth in using the care team model. State level details for practice model distribution, provider workforce measures, and SOP for years 2010 and 2019 are presented in Appendix A.
• Estimating Practice Model Utilization. Table 2 presents the odds ratios from the logistic model used to estimate practice model share with physician anesthesiologist alone versus care team and undirected CRNA versus care team being the included comparisons. The size of the total anesthesia provider workforce is significantly associated with reduced odds of the physician anesthesiologist-alone model (OR, 0.44; P < .0001). The odds for using the undirected CRNA model compared with the care team model are similar (OR, 0.48; P =.0533), although the result does not quite reach statistical significance. Similarly, an increase of one in the ratio of CRNAs to physician anesthesiologists is associated with much lower odds (OR, 0.30; P < .0001) of AA payment. This ratio is not related to the relative use of the undirected CRNA or care team models. Findings imply that the presence of additional CRNAs can fulfill the anesthesia care requirements, with less reliance on additional AAs. Furthermore, with a higher ratio of CRNAs to physician anesthesiologists, facilities may allocate their resources in a way that optimizes staffing and reduces the need for additional personnel. This approach can help control costs while ensuring the appropriate utilization of anesthesia providers.
The increased presence of AAs is also associated with reduced use of a physician anesthesiologist-alone model compared with the care team (OR, 0.90; P <.0001) while having no significant effect on the other comparison (OR, 0.96; P = .1764). Relative to the presence of a supervision requirement in a state, having no CRNA SOP restrictions increases the odds of the anesthesiologistalone model (OR, 1.92; P = .0052) while having no statistically significant effect at the standard P < .05 level on the undirected CRNA model (OR, 2.05; P = .0897) relative to use of the care team model.
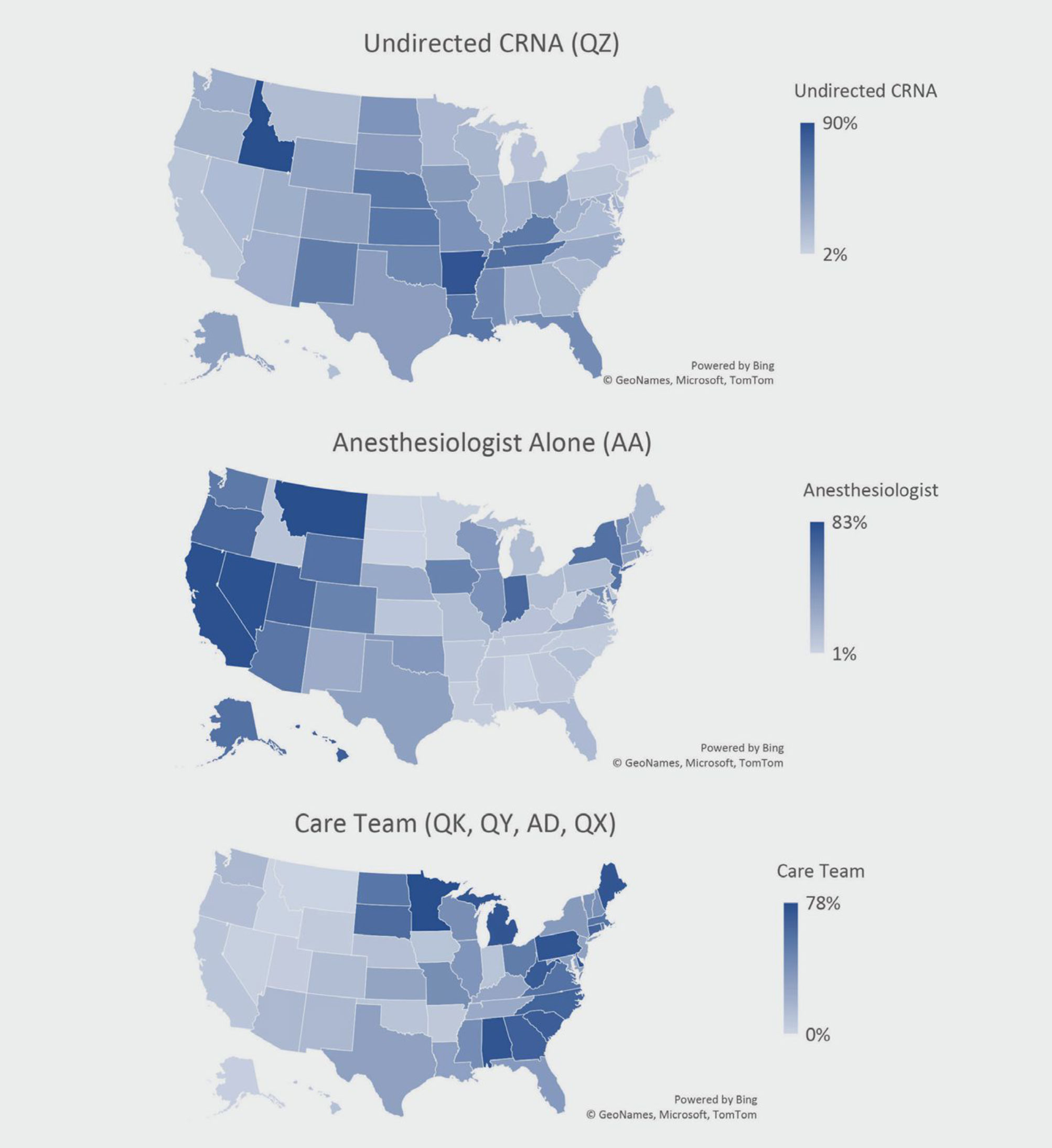
Figure 2. Share of Medicare Payments by Practice Model, 2019
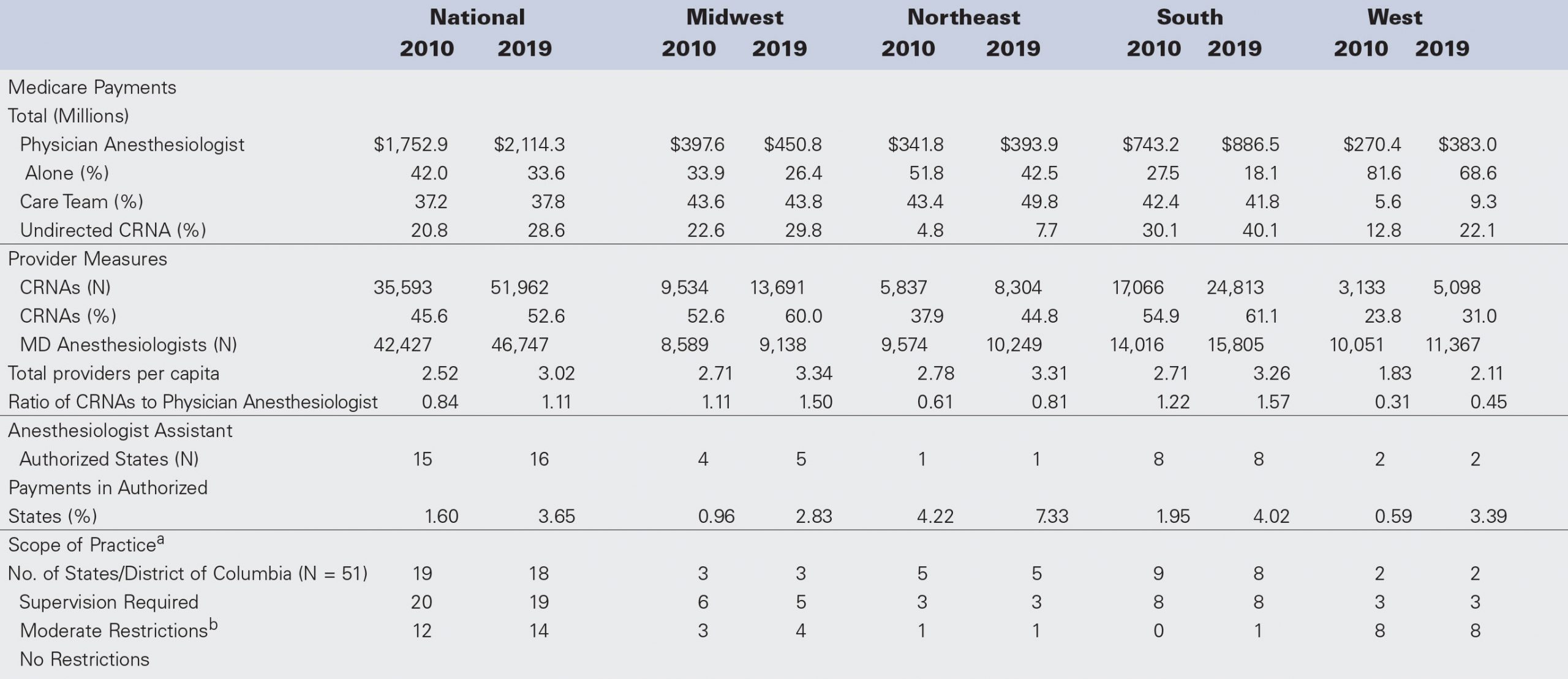
Table 1. Medicare Payments by Practice Model, Workforce Composition, and Scope of Practice Measures, 2010 and 2019 aBased on nursing and/or inpatient hospital regulations. Changes to SOP include Minnesota (direction/collaboration removed in 2014), Delaware (supervision removed in 2014), and Kentucky (opted out in 2012 and removed direction/collaboration in 2018).
Moderate restrictions include federal supervision and/or state direction/collaboration.
Abbreviations: CRNA, certified registered nurse anesthetist; SOP, scope of practice.
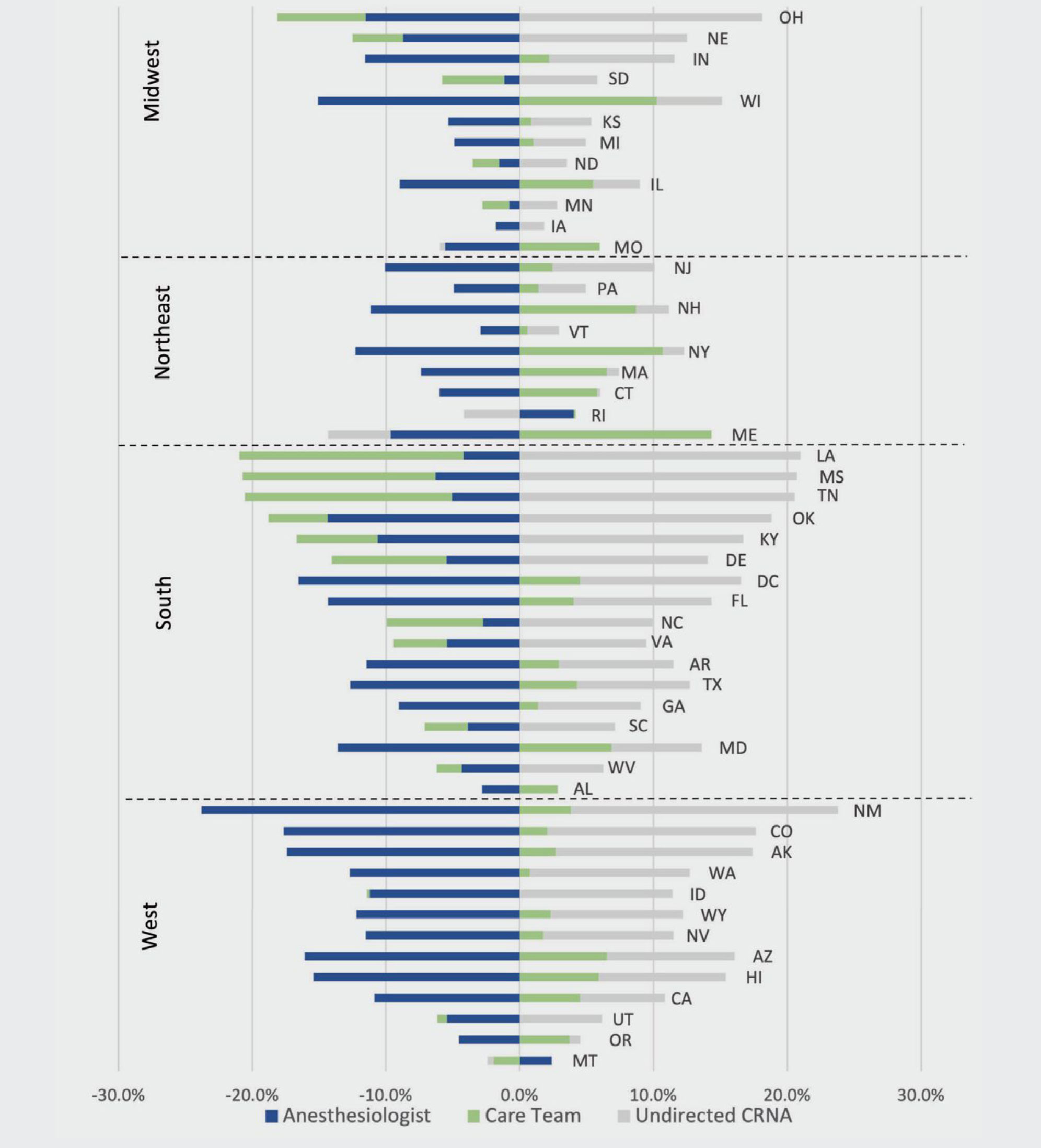
Figure 3. 2010-2019 Change in Anesthesia Delivery Model Share
Abbreviation: CRNA, certified registered nurse anesthetist
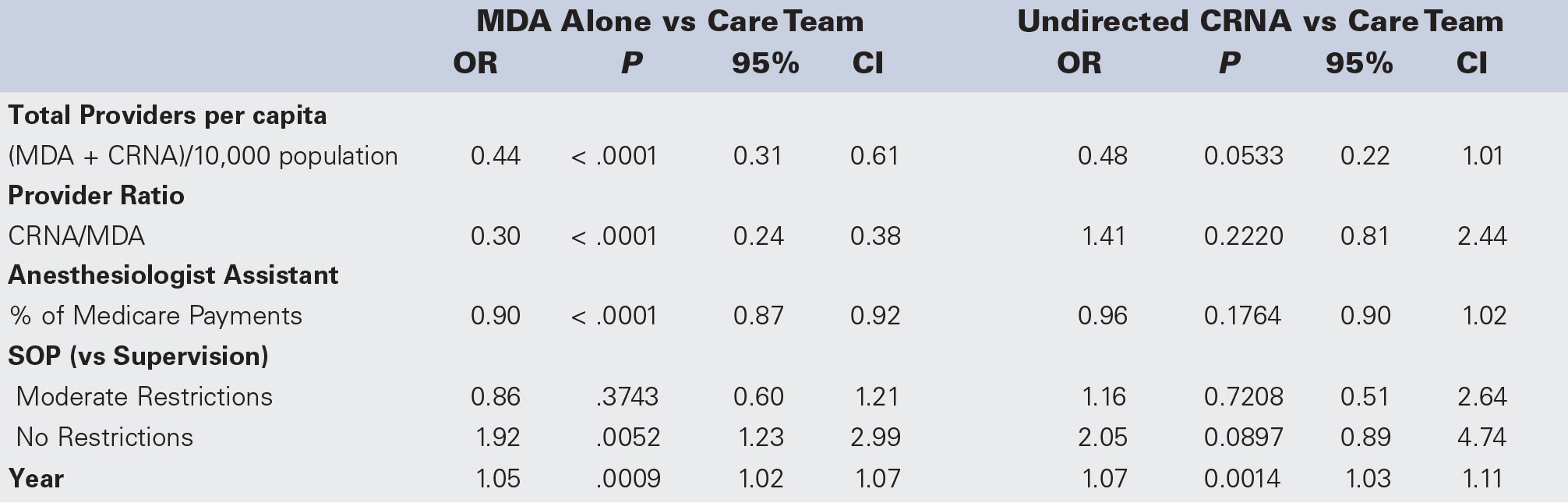
Table 2. Multinomial Logistic Regression of State Anesthesia Practice Model Payment Share, 2010-2019
Abbreviations: CRNA, certified registered nurse anesthetist; MDA, physician anesthesiologist; CI, confidence interval; SOP, scope of practice
The presence of collaboration or direction requirements is not signifi cantly associated with a practice model for either comparison. The year variable is positively associated with greater use of both the physician anesthesiologist alone and undirected models compared with the care team, suggesting that over those 10 years, the use of the non-care team models increased. This includes increased use of the physician anesthesiologist-alone model after accounting for shifts in the labor force and state SOP laws, which tended to favor CRNA-centric models.
Deviations for each state from their expected share of physician anesthesiologist alone, care team, and undirected CRNA payments, after adjusting for the covariates in the model, are plotted in Figure 4. The model explains the variation in the use of the physician anesthesiologist-alone model quite well, with only six states falling more than 10 percentage points from their expected value. However, there are clear regional differences, with respect to each of the other practice model types. In the CRNA-centric models, clear region patterns are apparent. All northeastern states deviate higher than their expected share of the care team and, except for New Hampshire, lower than their expected share of undirected CRNA payments. Rhode Island and Connecticut have the most extreme deviations in both model types. Deviations are smaller in western states, with most states within 10 points of their expected values. In the midwest and south, some states have large deviations from expected in both the care team and undirected CRNA models, with some over 20 points. Minnesota, Michigan, Delaware, Virginia, West Virginia, and South Carolina all have shares of care team payments that are significantly higher than expected. In contrast, Nebraska, Kansas, Arkansas, Tennessee, Louisiana, Oklahoma, and Florida all have shares of undirected CRNA payments that are substantially above their expected values.
DISCUSSION
The findings of this study suggest that over the past 10 years, anesthesia delivery models have shifted toward greater efficiency but at an uneven rate. This trend to increased use of undirected CRNAs is most apparent in the south and west, while the magnitude of change in the northeast and midwest, has been smaller. The increasing use of the undirected CRNA model can be interpreted in multiple ways. First, the anesthesia labor force has shifted substantially over the past 10 years from 54.1% physicians in 2010 to 52.6% CRNAs in 2019. This shift is most clearly illustrated in the significant decline across virtually all states in the share of payments for physicianonly anesthesia services in favor of increased use of CRNAs, both in a care team as well as undirected.
The results also suggest that greater provider availability per capita is necessary to support a care team model. Western states with lower total anesthesia providers per 10,000 population are most likely to use independent or undirected anesthesia delivery models, while midwestern and southern states such as Michigan, Minnesota, Alabama, and West Virginia have much greater overall provider availability and the care team is dominant. However, the effects of workforce composition are not the only important findings. Results from the multivariate analysis find that the presence of a supervision requirement and contributions from AAs are both associated with greater use of the care team over the physician anesthesiologist-alone model while these factors are not associated with use of the undirected CRNA model positively or negatively. This suggests that regulatory restrictions or the presence of AAs, which both necessarily encourage more intense involvement of physicians in team-based care, also may discourage the use of the physician anesthesiologist-alone model.
After model adjustment, there remains a statistically significant increasing trend toward the using of noncare team models, both physician anesthesiologist alone and undirected CRNA. The positive finding for physician anesthesiologist alone is somewhat puzzling given the overall trend, but perhaps makes sense when the supply of CRNAs is held constant. Without an increasing supply of CRNAs, greater use of the care team is not possible, and we are left with both types of providers practicing outside a medically directed or care team model. This finding underscores the importance of considering the effects of practice model choice when assessing whether there is a provider shortage in anesthesia. An excess demand for CRNAs to work in a restricted care team may not indicate a true shortage but rather the presence of an inefficient and overly restricted workforce. In the west, where use of the care team model is much less common relative to other regions, the density of anesthesia providers is much lower compared with regions where it is heavily used. There has been speculation about provider shortages in recent years with some acknowledgment that these estimates are sensitive to the level of substitution assumed among various types of health professions performing the same tasks. Accordingly, greater use of undirected and independent CRNA practice in care team-dominant regions would increase productivity from the existing provider workforce and lessen any apparent shortage.
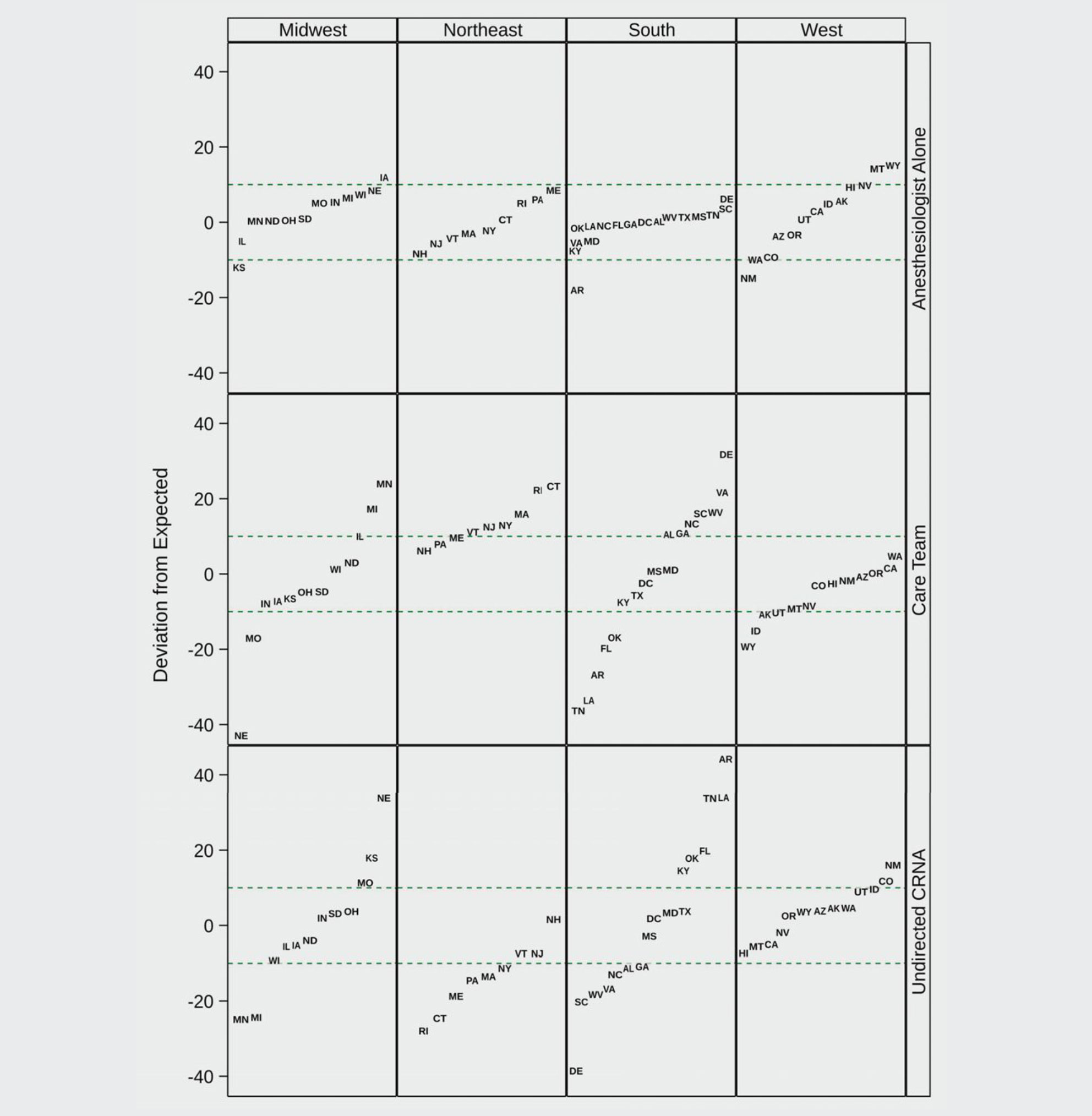
Figure 4. State Deviations from Predicted Share of Payments by Model and Region, 2019
Abbreviation: CRNA, certified registered nurse anesthetist
While it is difficult to quantify precisely, hospitals may adopt more flexible anesthesia delivery models that use higher ratios of CRNAs to physician anesthesiologists in response to economic pressures, given that physician anesthesiologist salaries can be double that of CRNAs. Evidence has demonstrated substantial excess costs attributable to medical direction and physicianonly models. However, using a physician anesthesiologist personally performing procedures is still common in certain settings and geographic areas. In this case, moving toward a team-based model of one physician to two or three CRNAs could represent a meaningfully improved cost-effectiveness. However, many regions of the country have long incorporated a team-based approach in anesthesia delivery. In these settings, increasing costefficiency involves shifting to less restrictive supervision-based teams of one physician anesthesiologist to five CRNAs or more. One study in an oncology setting suggests that the shift from 1:2 to 1:3 can save 12% to 14% in anesthesia costs, while a 1:6 model could save 24% to 29%.13 It follows then that the most cost-effective model is a CRNA-only model with no excess cost attributable to physician supervision or direction. Potentially, this model saves an additional 25% over a supervision model
or 40% over a 1:3 direction model.2 This model is already commonly used in smaller and rural hospitals and if used more widely, anesthesia labor costs could be reduced up to an estimated 38%.
Practice consolidation, including the acquisition of many anesthesiology practices by large national practice groups, could drive greater use of undirected CRNAs along with Medicare billing of QZ due to improved labor force efficiency and simpler administration and documentation requirements. Recent trends have seen significant consolidation in provider group practices, including anesthesia and facilities offering surgical care. These mergers are mainly driven by a desire to increase scale and negotiate leverage with payors but also have implications for the organization of anesthesia service delivery. Larger organizations have higher overhead and management costs, making efficient service delivery much more important. If the same organization employs both the physician anesthesiologist and the CRNA, administrative simplicity favors QZ eliminating documentation requirements for medical direction. While some physician anesthesiologists may prefer billing medical direction, even under Medicare, for purposes of documenting their participation in the case,14 the organizational shifts occurring in group practice ownership and facility policies seem to encourage the opposite. Alternative approaches to delivering anesthesia are those that use CRNAs practicing at their full scope while collaborating with physicians in a way that eliminates duplication of services and makes the best use of the skills and training of all providers. These models allow flexibility for facilities to use their anesthesia providers in the most cost-effective manner to meet the community’s needs.
• COVID-19 Impact on CRNA Practice. The data analyzed in this study did not capture the year 2020 when the COVID-19 pandemic dramatically impacted the delivery of healthcare services including surgical care and critical care nursing services. Federal and state executive orders removing barriers to CRNA SOP may ultimately be shown to have longer-term impacts on supervision policies, CRNA practice, and the division of labor among teams of providers within facilities. Recent studies have demonstrated that the COVID-19 crisis expanded roles for many CRNAs, particularly those where state level executive orders removed barriers to full SOP.15 Given the opportunity to adopt new models of practice without regulatory restrictions on nurses, facilities may decide that these new care delivery models serve them well and keep them beyond the COVID-19 crisis.
• Limitations. The QZ modifier is a direct measure of billing practices only. Interpreting any larger shift in practice models must be done with caution because Medicare represents only one of many payors with only one set of rules that may be interpreted as particularly friendly to CRNAs. The results of this analysis include only Medicare Part B reimbursements, which reflects only a subset of all Medicare reimbursements. It does not include Medicare Advantage payments or the cost-based nurse anesthesia pass-through funding available under Part A for eligible rural facilities. Medicare Advantage has variable penetration across states with reimbursement regulations not determined by CMS policy but by commercial carriers offering those policies. Higher penetration of Medicare Advantage potentially allows commercial payors greater influence in determining practice models in that market. Conversely, a high level of Part A pass-through funds obscures a state’s overall share of undirected CRNA services. States with large shares of hospitals eligible for this funding may present as having lower shares of undirected CRNA payments than would otherwise be observed if all Medicare payments were included in the analysis. Likewise, at a state level, the observed practice model distributions cannot be assumed representative of all care in the state, and providers may vary their billing practices according to the regulations of more predominant payors. As previously discussed, commercial and Medicaid reimbursement policies can differ in how CRNA services are (or are not) reimbursed and thus may present differently from Fee-for-Service Medicare and have divergent impacts on practice models.
CONCLUSION
Policy experts have long puzzled over how to best deliver high-quality healthcare at a lower cost, increasing the value for patients while improving access to care for vulnerable populations. To move toward improved costeffectiveness in anesthesia delivery, it is critical to identify the structures and processes by which inefficiency is incentivized under the current system. These may include state regulatory barriers or facility rules that prevent CRNAs from practicing at the top of their license and discriminatory reimbursement policies.
The healthcare system has experienced a significant movement toward expanded SOP for non-physician providers including, in anesthesia. The increased use of QZ billing for undirected CRNA services suggests a broader scope of practice for CRNAs with less physician involvement than a traditional medical direction model. Incremental modifications to SOP laws have supported the shift toward undirected CRNAs. Since 2019, more states have reduced CRNA SOP barriers, including Arkansas, Arizona, and Oklahoma, which were already well above their expected share of undirected CRNA Medicare reimbursement based on the current analysis. Michigan, with one of the most CRNA-dominant anesthesia labor forces in all states, in 2021 also removed its requirement for physician supervision. Many more states and facilities altered policies in response to COVID-19, with the long-term impact of these changes still unknown. Yet, as we move beyond the COVID-19 era, entrenched opposition to full SOP for CRNAs remains in many facilities and state regulatory bodies. In a market-oriented healthcare system such as in the United States, we should strive for policies that encourage fair competition among providers who provide equivalent high-quality services.
REFERENCES
1. Cintina I, Hogan P, Schroeder C, Simonson B, Quraishi J. Cost Effectiveness of Anesthesia Providers and Implications of Scope of Practice in a Medicare Population. Nurs Econ. 2018;36(2):67-73.
2. Hogan PF, Seifert RF, Moore CS, Simonson BE. Cost effectiveness analysis of anesthesia providers. Nurs Econ. 2010;28(3):159–169.
3. Hoyem RL, Quraishi JA, Jordan L, Wiltse Nicely KL. Advocacy, Research, and Anesthesia Practice Models: Key Studies of Safety and Cost-Effectiveness. Policy Polit Nurs Pract. 2019;20(4):193-204. doi:10.1177/1527154419874410
4. Mills A, Sorensen A, Gillen E, et al. Quality, Costs, and Policy: Factors Influencing Choice of Anesthesia Staffing Models. J Healthc Manag. 2020;65(1):45-60. doi:10.1097/JHM-D-18-00186
5. Quraishi JA, Jordan LM, Hoyem R. Anesthesia Medicare trend analysis shows increased utilization of CRNA services. AANA J. 2017;85(5):375-383.
6. https://www.bls.gov/oes/current/oes291151.htm#nat 7. https://www.bls.gov/oes/current/oes291211.htm#st
8. Coomer N, Mills A, Beadles C, Gillen E, Chew R, Quraishi J. Anes- thesia Staffing Models and Geographic Prevalence Post-Medicare CRNA/Physician Exemption Policy. Nurs Econ. 2019;37(2):86-91.
9. Liao CJ, Quraishi JA, Jordan LM. Geographical Imbalance of Anes- thesia Providers and its Impact on the Uninsured and Vulnerable Populations. Nurs Econ. 2015;33(5):263-270.
10. Martsolf GR, Baird M, Cohen CC, Koirala N. Relationship Between State Policy and Anesthesia Provider Supply in Rural Communities. Med Care. 2019;57(5):341-347. doi:10.1097/MLR.0000000000001106 11. https://issuu.com/aanapublishing/docs/scope_of_nurse_anes- thesia_practice _2.23?fr-sNDg2MDU2NDAxMjU
12. IHS Markit Ltd. The Complexities of Physician Supply and Demand: Projections From 2019 to 2034. AAMC; 2021. https://www.aamc.org/ media/54681/download
13. French KE, Guzman AB, Rubio AC, Frenzel JC, Feeley TW. Value based care and bundled payments: Anesthesia care costs for out- patient oncology surgery using time-driven activity-based costing. Healthcare. 2016;4(3):173–180. doi:10.1016/j.hjdsi.2015.08.007
14. Byrd JR, Merrick SK, Stead SW. Billing for Anesthesia Services and the QZ Modifier: A Lurking Problem. ASA Monitor. 2011;75(6):36-38. 15. Everson M, Wilbanks BA, Hranchook AM, et al. From the Operating Room to the Front Lines: Shared Experiences of Nurse Anesthetists During the Coronavirus Pandemic. AANA J. 2021;89(2):109-116.
AUTHORS
Ruby L. Hoyem, PhD, was a Research Associate at the American Association of Nurse Anesthesiology, Rosemont, Illinois.
Lorraine Jordan, PhD, CRNA, CAE, FAAN, is AANA Chief Science and Practice Officer and AANA Foundation CEO, American Association of Nurse Anesthesiology, Rosemont, Illinois. Email: ljordan@aana.com
Valentina V. Lukyanova, PhD, is a Research Associate at the American Association of Nurse Anesthesiology, Rosemont, Illinois. Email: vlukyanova@aana.com
Trinidad Legaspi, JD, LLM, is Director of Research, Quality and Strategic Policy at the American Association of Nurse Anesthesiology, Rosemont, Illinois. Email: tlegaspi@aana.com
DISCLOSURES
Name: Ruby L. Hoyem, PhD
Contribution: This author made significant contributions to the conception, synthesis, writing, and final editing and approval of the manuscript to justify inclusion as an author.
Disclosures: None.
Name: Lorraine Jordan, PhD, CRNA, CAE, FAAN
Contribution: This author made significant contributions to the conception, synthesis, writing, and final editing and approval of the manuscript to justify inclusion as an author.
Disclosures: None.
Name: Valentina V. Lukyanova, PhD
Contribution: This author made significant contributions to the conception, synthesis, writing, and final editing and approval of the manuscript to justify inclusion as an author.
Disclosures: None.
Name: Trinidad Legaspi, JD, LLM
Contribution: This author made significant contributions to the conception, synthesis, writing, and final editing and approval of the manuscript to justify inclusion as an author.
Disclosures: None.
Copyright of AANA Journal is the property of American Association of Nurse Anesthetists and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder’s express written permission. However, users may print, download, or email articles for individual use.
